Telehealth has evolved from a concierge convenience for private insurance companies into an essential tool for increasing access to care1 and improving health equity.2 The benefits and challenges of telehealth and telementoring are documented below, as are recommendations for policymakers to consider to improve individuals’ access to care.
Telehealth Solutions
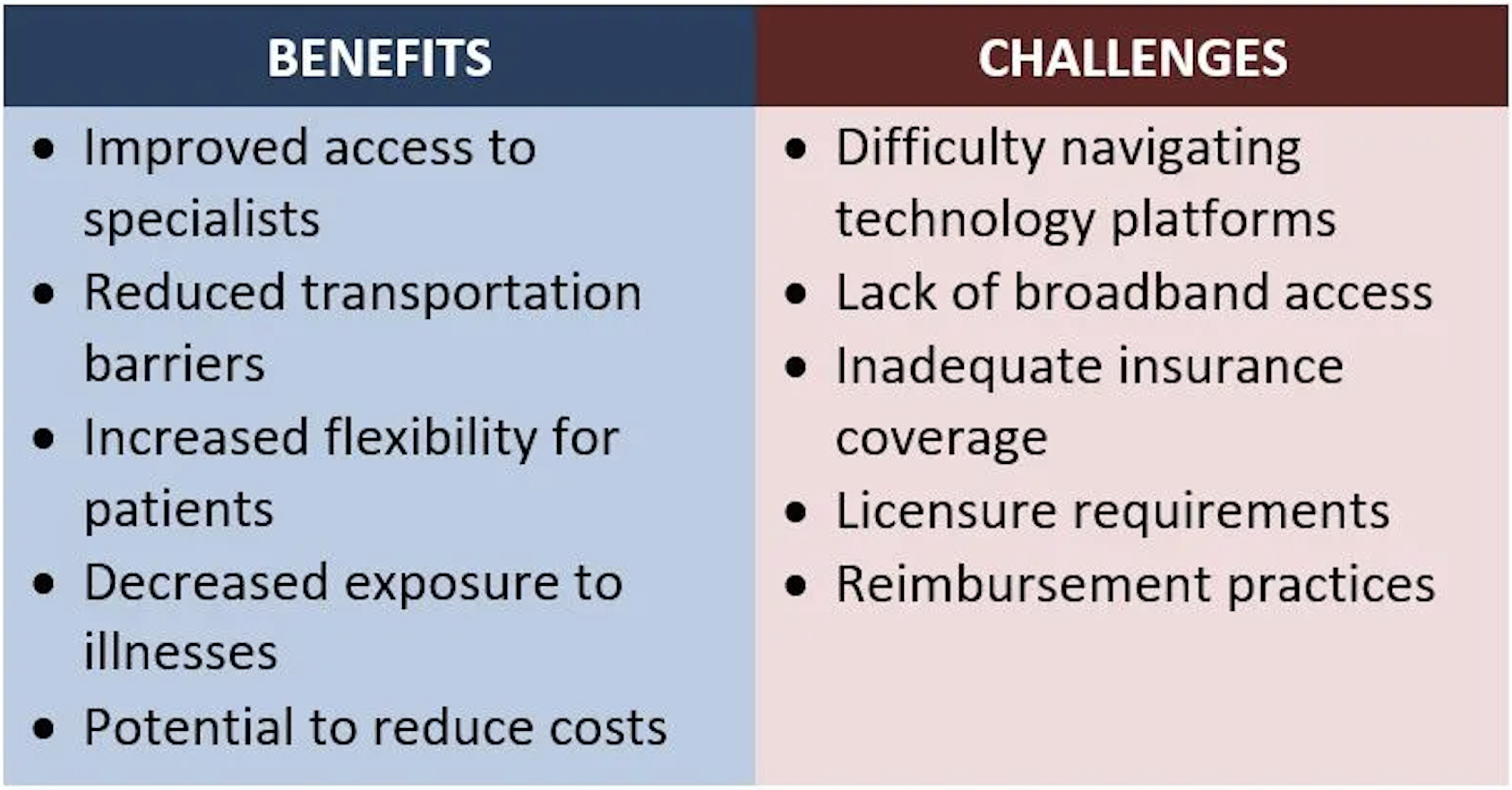
The COVID-19 Public Health Emergency, which ended in May 2023, expanded access to telehealth and created an opportunity to examine telehealth’s use, impact, and costs during the pandemic. Although some of the efforts to understand telehealth in the context of COVID-19 are ongoing, there are documented challenges and benefits to consider when offering telehealth services.
Improving Access To Care Via Telehealth
Telehealth can help patients by improving the patient experience and removing barriers to care. The flexibility provided through telehealth is particularly beneficial for individuals with disabilities and chronic health concerns. Combining telehealth services with community support and investments in workforce development can also further address the needs of patients and providers in rural communities.
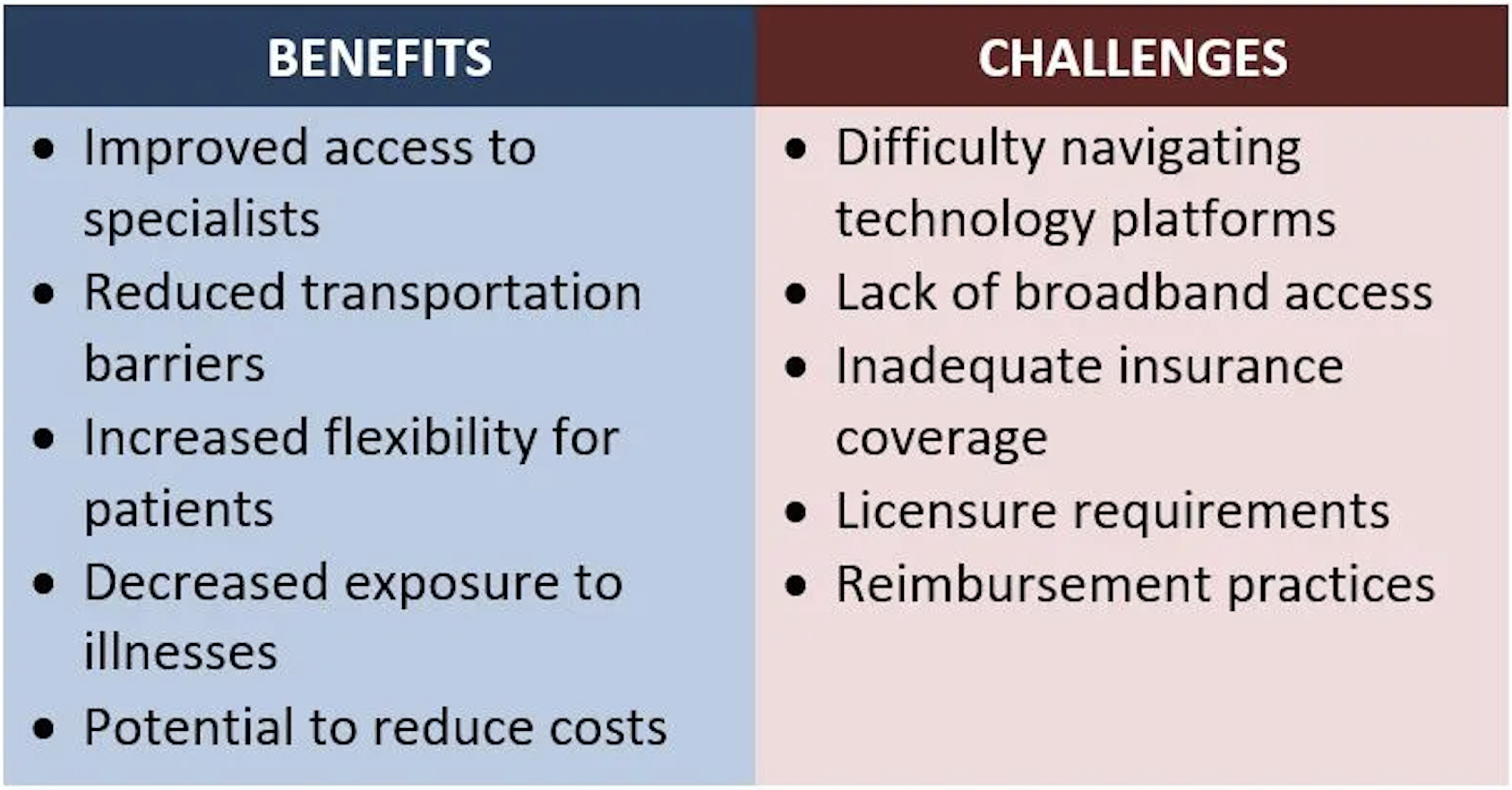
- PATIENT EXPERIENCE: Telehealth visits provide flexibility for patients and minimize transportation barriers (e.g., long travel times, parking expenses, delays in public transportation) to accessing care. Patients miss less school or work3 for appointments and parents have fewer childcare burdens to receive care for themselves. Using telehealth for appointments also reduces exposure to illness, which is particularly important for patients who are immunocompromised.
- TECHNOLOGY NAVIGATION: The format of telehealth appointments varies based on patients’ needs. If a visual assessment of the patient is not required, telehealth can be delivered by telephone; otherwise, patients and providers need access to strong, reliable internet connection with voice and video capabilities. In areas with limited internet access, telehealth rooms could be established in the community, such as in local pharmacies, libraries, or schools. Telehealth delivery through telephone may be especially useful for patients in rural and older communities as it eliminates video-related barriers.
- MENTAL HEALTH CARE: Telehealth has been particularly effective at increasing access to mental health care.4 Telebehavioral health care delivery also has applications outside of health care settings. For example, it is a promising option to support students in schools when in-person mental health support is unavailable.
Suitability Of Telehealth Visits
In many instances, in-person interactions are not required for diagnosis or care delivery. Certain specialized healthcare roles (e.g., genetic counselors, nutritionists, diabetes educators) can effectively provide personalized education and recommendations without in-person visits. This can also extend to provider specializations (e.g., endocrinology) where patient history and labs are more informative than a physical examination. Telehealth can also be used to deliver routine primary care services, such as medication counseling, referral requests, and follow-up after labs or imaging. However, some specialties (e.g., dermatology, orthopedics, cardiology, pulmonology) are currently not well suited for telehealth when hands-on physical assessments are required. Telehealth can still be used in these specialties for medication management.
Financial And Human Capital Considerations
- STAFFING: Telehealth has been associated with decreased staffing costs and improved physician recruitment and retention, particularly in rural areas.
- REPLACING IN-PERSON VISITS: A systematic review5 of studies that assessed telehealth use during the early months of the pandemic suggests telehealth visits replaced in-person visits and were not an additive service. Similarly, an evaluation of telehealth adoption at Duke Health System (July 2019 to October 2020) found the total number of patient visits remained steady, but the modality of visits (in person vs telehealth) changed with some specialties. For example, there was a notable switch from in-person to telehealth visits for psychiatric care.
- EFFICIENCY & SAVINGS: Reducing or eliminating travel for appointments can save patients time and money. Additionally, patients with transportation barriers may be more likely to seek care via telehealth. Without this access, they may delay care until their health worsens, which can be costly and negatively impact health outcomes.[1]
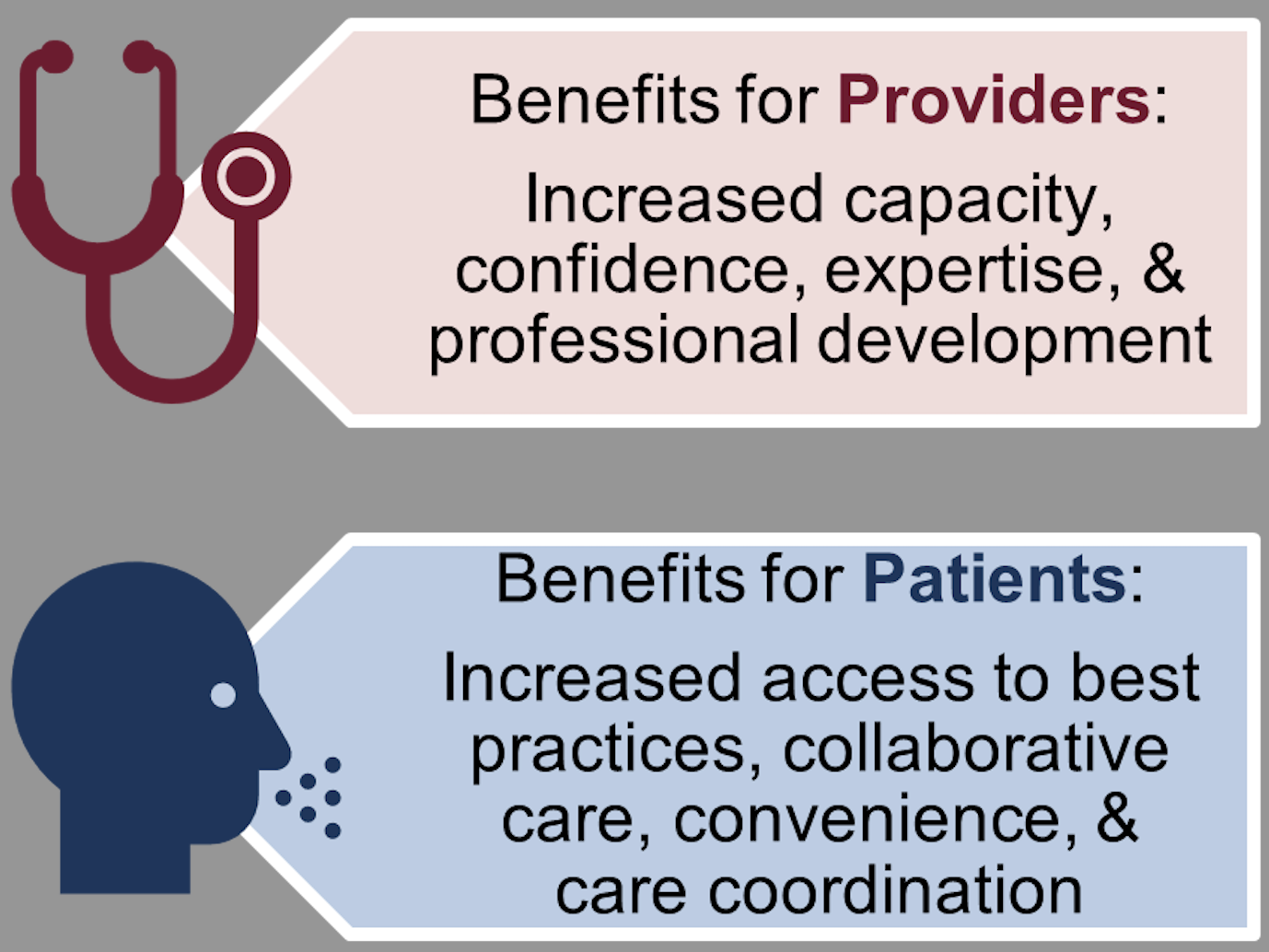
Supporting the Needs of Providers: Benefits of Telementoring
The use of virtual approaches in health care can be beneficial not only for patients, but for providers as well. Telementoring is a collaborative learning approach designed to expand the capacity of primary care providers to help patients receive the care they need, when they need it. The model can increase providers’ knowledge and confidence, while reducing professional isolation. This equips providers to deliver best-practice specialty care and reduce health disparities.
Telementoring is distinct from telemedicine in that specialists do not assume the care of the patient. Instead, primary care providers collaborate with specialists to share their expertise, best practices, and experience while discussing de-identified cases. Over time, frontline providers become experts—engaged in a wider community of learners and empowered to address complex conditions or situations in their local communities. With telementoring, primary care providers are supported by specialists (for advice and referrals). This creates an effective triage system and direct linkage to care where patients gain access to best practices and collaborative care close to home, which is particularly critical in rural areas.
Example: Project Echo’s Telementoring Model
Project ECHO enables providers to rapidly transfer knowledge and exponentially increase capacity to deliver best-practice care to underserved populations. The model’s approach creates an infrastructure for knowledge sharing in rural and underserved communities globally. Providers become more independent as their skills, confidence, and self-efficacy grow.
Key components of the model include using technology to leverage scarce resources, sharing best practices to reduce disparities, using case-based learning to master complexity, and monitoring outcomes to increase impact.
Policy Recommendations to Improve Access to Care
Remove Barriers For Telehealth Provision
Lack of clarity regarding the reimbursement of telehealth services has delayed providers and health systems from making long-term investments in telemedicine technology. Additionally, variation in state laws and system policies can result in significant differences in whether and how telehealth is delivered across state lines. Payment policies can also impact access to telehealth services. One study found that adults in states with payment parity laws were 23% more likely to use telehealth services than those in nonparity states. In addition, easing provider licensure burdens to practice interstate could expand patients’ choice of providers and facilitate access to telehealth services. One example includes multi-state compacts, which streamline the licensing process for providers seeking to practice interstate.
Evaluate Telehealth Utilization, Costs, & Benefits
Analyzing data on telehealth use and associated factors (e.g., cost, benefits) can provide insights to assess telehealth’s impact and better understand potential differences across specialties, locations, demographics, and socioeconomic factors. The results of such an evaluation could identify gaps and strengths related to the access, use, and implementation of telehealth service delivery models and inform future interventions.
Expand Access To Telehealth Solutions
Telehealth has the potential to improve health equity, but it is not a complete panacea. During the pandemic, telehealth usage was more common in urban areas, among those with higher incomes, and young-to-middle aged individuals, indicating an opportunity to expand access for other populations. Broadband access – one of the biggest barriers to adoption in rural and low-income communities – as well as insurance coverage are important predictors of telehealth access.
Consider Capacity
- Leverage Community Partners & Health Professionals. To expand access to care in areas with primary care provider shortages, telehealth rooms could be established in convenient community locations and staffed with community health workers. These health professionals can help patients navigate telehealth technology and communicate with providers. In circumstances where physical examinations are required, registered nurses could conduct the assessments and relay findings to a telehealth provider.
- Bolster the capacity of primary care provider networks. Efforts to enhance providers’ knowledge, confidence, and connection to professional networks may help combat provider burnout as well as support their confidence and expertise. At the state level, some states have used Medicaid funds to support Project ECHO. Example: New Mexico’s approved 1115 waiver requires its Medicaid managed care organizations (MCOs) to support the project, aiming to improve access to care and reduce costs.
[1] One study of a multidisciplinary clinic for heart disease prevention found telehealth visits improved patient compliance, blood pressure, and cholesterol. Another study found that while total visit numbers for diabetes management increased when a practice expanded telehealth access, patients also had better blood sugar control and optimized insulin dosing compared to in-person visits only.
End Notes / References
- Shah et al. (2022). Exploring the role of telehealth in providing equitable healthcare to the vulnerable patient population during Covid-19. Journal of Telemedicine and Telecare, 1357633X2211137.
- Anaya et al. (2022). Post-pandemic telehealth policy for primary care: An equity perspective. The Journal of the American Board of Family Medicine, 35(3), 588–592.
- Polinski et al. (2015). Patients’ satisfaction with and preference for telehealth visits. Journal of General Internal Medicine, 31(3), 269–275.
- Schaffer et al. (2020). Telemental health care: A review of efficacy and interventions. Telehealth and Medicine Today.
- Harju, A., & Neufeld, J. (2022). Telehealth utilization during the COVID-19 pandemic: A preliminary selective review. Telemedicine Reports, 3(1), 38–47.
- Drake et al. (2022). Understanding telemedicine’s “new normal”: Variations in telemedicine use by specialty line and patient demographics. Telemedicine and e-Health, 28(1), 51–59.
- Project ECHO. (n.d.). Project ECHO: Using technology, not proximity, to connect and share knowledge. PennState Clinical and Translational Science
The Research-to-Policy Collaboration (RPC) works to bring together research professionals and public officials to support evidence-based policy. Please visit their website to learn more.
Key Information
RPC Website
Research-to-Policy Collaboration
More RPC Resources
RPC Resources
Publication DateJuly 11, 2023
Resource TypeWritten Briefs
Share This Page
Telehealth has evolved from a concierge convenience for private insurance companies into an essential tool for increasing access to care1 and improving health equity.2 The benefits and challenges of telehealth and telementoring are documented below, as are recommendations for policymakers to consider to improve individuals’ access to care.
Telehealth Solutions
The COVID-19 Public Health Emergency, which ended in May 2023, expanded access to telehealth and created an opportunity to examine telehealth’s use, impact, and costs during the pandemic. Although some of the efforts to understand telehealth in the context of COVID-19 are ongoing, there are documented challenges and benefits to consider when offering telehealth services.
Improving Access To Care Via Telehealth
Telehealth can help patients by improving the patient experience and removing barriers to care. The flexibility provided through telehealth is particularly beneficial for individuals with disabilities and chronic health concerns. Combining telehealth services with community support and investments in workforce development can also further address the needs of patients and providers in rural communities.
- PATIENT EXPERIENCE: Telehealth visits provide flexibility for patients and minimize transportation barriers (e.g., long travel times, parking expenses, delays in public transportation) to accessing care. Patients miss less school or work3 for appointments and parents have fewer childcare burdens to receive care for themselves. Using telehealth for appointments also reduces exposure to illness, which is particularly important for patients who are immunocompromised.
- TECHNOLOGY NAVIGATION: The format of telehealth appointments varies based on patients’ needs. If a visual assessment of the patient is not required, telehealth can be delivered by telephone; otherwise, patients and providers need access to strong, reliable internet connection with voice and video capabilities. In areas with limited internet access, telehealth rooms could be established in the community, such as in local pharmacies, libraries, or schools. Telehealth delivery through telephone may be especially useful for patients in rural and older communities as it eliminates video-related barriers.
- MENTAL HEALTH CARE: Telehealth has been particularly effective at increasing access to mental health care.4 Telebehavioral health care delivery also has applications outside of health care settings. For example, it is a promising option to support students in schools when in-person mental health support is unavailable.
Suitability Of Telehealth Visits
In many instances, in-person interactions are not required for diagnosis or care delivery. Certain specialized healthcare roles (e.g., genetic counselors, nutritionists, diabetes educators) can effectively provide personalized education and recommendations without in-person visits. This can also extend to provider specializations (e.g., endocrinology) where patient history and labs are more informative than a physical examination. Telehealth can also be used to deliver routine primary care services, such as medication counseling, referral requests, and follow-up after labs or imaging. However, some specialties (e.g., dermatology, orthopedics, cardiology, pulmonology) are currently not well suited for telehealth when hands-on physical assessments are required. Telehealth can still be used in these specialties for medication management.
Financial And Human Capital Considerations
- STAFFING: Telehealth has been associated with decreased staffing costs and improved physician recruitment and retention, particularly in rural areas.
- REPLACING IN-PERSON VISITS: A systematic review5 of studies that assessed telehealth use during the early months of the pandemic suggests telehealth visits replaced in-person visits and were not an additive service. Similarly, an evaluation of telehealth adoption at Duke Health System (July 2019 to October 2020) found the total number of patient visits remained steady, but the modality of visits (in person vs telehealth) changed with some specialties. For example, there was a notable switch from in-person to telehealth visits for psychiatric care.
- EFFICIENCY & SAVINGS: Reducing or eliminating travel for appointments can save patients time and money. Additionally, patients with transportation barriers may be more likely to seek care via telehealth. Without this access, they may delay care until their health worsens, which can be costly and negatively impact health outcomes.[1]
Supporting the Needs of Providers: Benefits of Telementoring
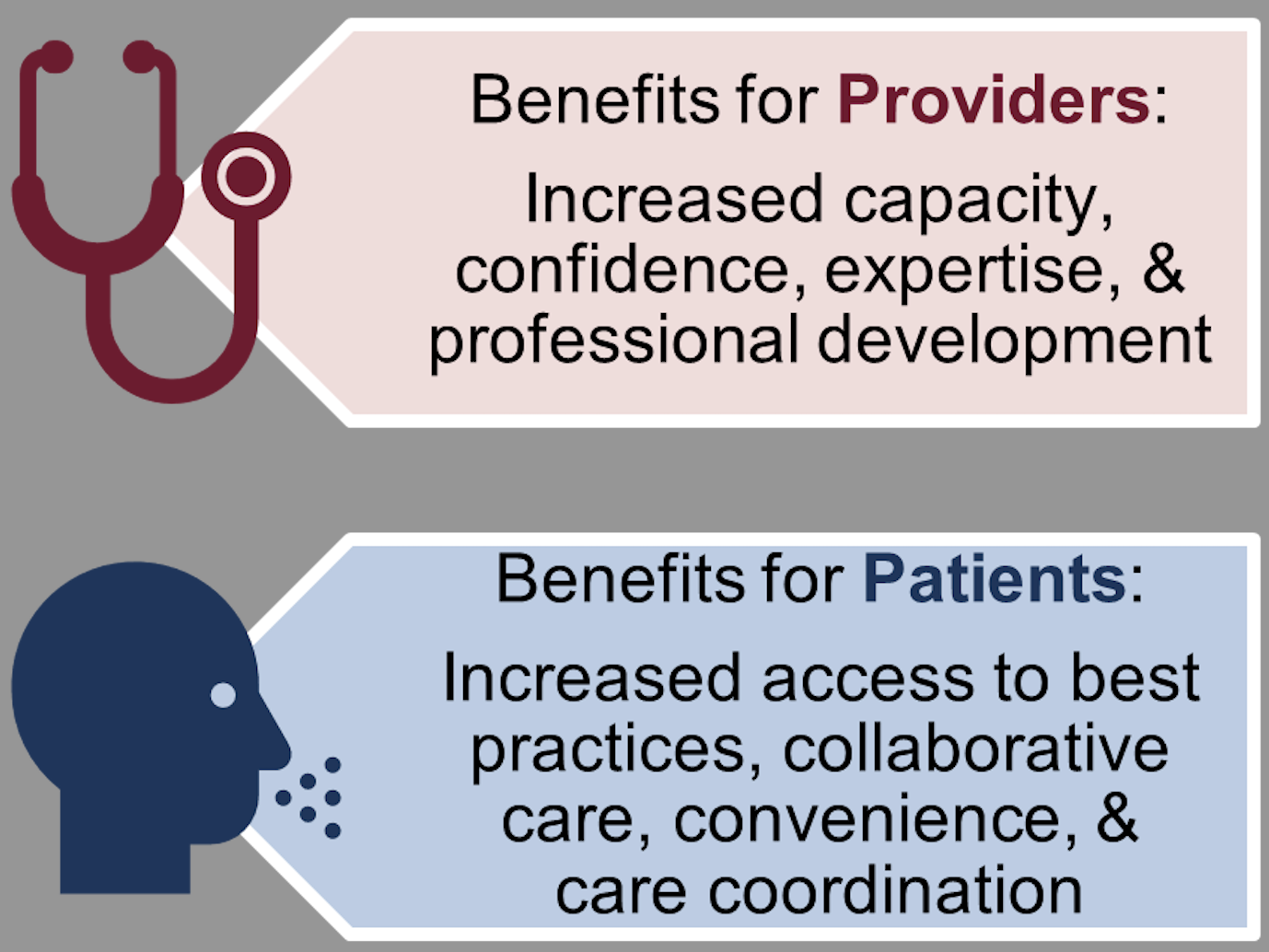
The use of virtual approaches in health care can be beneficial not only for patients, but for providers as well. Telementoring is a collaborative learning approach designed to expand the capacity of primary care providers to help patients receive the care they need, when they need it. The model can increase providers’ knowledge and confidence, while reducing professional isolation. This equips providers to deliver best-practice specialty care and reduce health disparities.
Telementoring is distinct from telemedicine in that specialists do not assume the care of the patient. Instead, primary care providers collaborate with specialists to share their expertise, best practices, and experience while discussing de-identified cases. Over time, frontline providers become experts—engaged in a wider community of learners and empowered to address complex conditions or situations in their local communities. With telementoring, primary care providers are supported by specialists (for advice and referrals). This creates an effective triage system and direct linkage to care where patients gain access to best practices and collaborative care close to home, which is particularly critical in rural areas.
Example: Project Echo’s Telementoring Model
Project ECHO enables providers to rapidly transfer knowledge and exponentially increase capacity to deliver best-practice care to underserved populations. The model’s approach creates an infrastructure for knowledge sharing in rural and underserved communities globally. Providers become more independent as their skills, confidence, and self-efficacy grow.
Key components of the model include using technology to leverage scarce resources, sharing best practices to reduce disparities, using case-based learning to master complexity, and monitoring outcomes to increase impact.
Policy Recommendations to Improve Access to Care
Remove Barriers For Telehealth Provision
Lack of clarity regarding the reimbursement of telehealth services has delayed providers and health systems from making long-term investments in telemedicine technology. Additionally, variation in state laws and system policies can result in significant differences in whether and how telehealth is delivered across state lines. Payment policies can also impact access to telehealth services. One study found that adults in states with payment parity laws were 23% more likely to use telehealth services than those in nonparity states. In addition, easing provider licensure burdens to practice interstate could expand patients’ choice of providers and facilitate access to telehealth services. One example includes multi-state compacts, which streamline the licensing process for providers seeking to practice interstate.
Evaluate Telehealth Utilization, Costs, & Benefits
Analyzing data on telehealth use and associated factors (e.g., cost, benefits) can provide insights to assess telehealth’s impact and better understand potential differences across specialties, locations, demographics, and socioeconomic factors. The results of such an evaluation could identify gaps and strengths related to the access, use, and implementation of telehealth service delivery models and inform future interventions.
Expand Access To Telehealth Solutions
Telehealth has the potential to improve health equity, but it is not a complete panacea. During the pandemic, telehealth usage was more common in urban areas, among those with higher incomes, and young-to-middle aged individuals, indicating an opportunity to expand access for other populations. Broadband access – one of the biggest barriers to adoption in rural and low-income communities – as well as insurance coverage are important predictors of telehealth access.
Consider Capacity
- Leverage Community Partners & Health Professionals. To expand access to care in areas with primary care provider shortages, telehealth rooms could be established in convenient community locations and staffed with community health workers. These health professionals can help patients navigate telehealth technology and communicate with providers. In circumstances where physical examinations are required, registered nurses could conduct the assessments and relay findings to a telehealth provider.
- Bolster the capacity of primary care provider networks. Efforts to enhance providers’ knowledge, confidence, and connection to professional networks may help combat provider burnout as well as support their confidence and expertise. At the state level, some states have used Medicaid funds to support Project ECHO. Example: New Mexico’s approved 1115 waiver requires its Medicaid managed care organizations (MCOs) to support the project, aiming to improve access to care and reduce costs.
[1] One study of a multidisciplinary clinic for heart disease prevention found telehealth visits improved patient compliance, blood pressure, and cholesterol. Another study found that while total visit numbers for diabetes management increased when a practice expanded telehealth access, patients also had better blood sugar control and optimized insulin dosing compared to in-person visits only.
End Notes / References
- Shah et al. (2022). Exploring the role of telehealth in providing equitable healthcare to the vulnerable patient population during Covid-19. Journal of Telemedicine and Telecare, 1357633X2211137.
- Anaya et al. (2022). Post-pandemic telehealth policy for primary care: An equity perspective. The Journal of the American Board of Family Medicine, 35(3), 588–592.
- Polinski et al. (2015). Patients’ satisfaction with and preference for telehealth visits. Journal of General Internal Medicine, 31(3), 269–275.
- Schaffer et al. (2020). Telemental health care: A review of efficacy and interventions. Telehealth and Medicine Today.
- Harju, A., & Neufeld, J. (2022). Telehealth utilization during the COVID-19 pandemic: A preliminary selective review. Telemedicine Reports, 3(1), 38–47.
- Drake et al. (2022). Understanding telemedicine’s “new normal”: Variations in telemedicine use by specialty line and patient demographics. Telemedicine and e-Health, 28(1), 51–59.
- Project ECHO. (n.d.). Project ECHO: Using technology, not proximity, to connect and share knowledge. PennState Clinical and Translational Science
The Research-to-Policy Collaboration (RPC) works to bring together research professionals and public officials to support evidence-based policy. Please visit their website to learn more.

Key Information
RPC Website
Research-to-Policy Collaboration
More RPC Resources
RPC Resources
Publication DateJuly 11, 2023
Resource TypeWritten Briefs
Share This Page
LET’S STAY IN TOUCH
Join the Evidence-to-Impact Mailing List
Keep up to date with the latest resources, events, and news from the EIC.