There is Good News. China has turned the curve on the coronavirus (no new cases as of 3/19/20); South Korea, Singapore, and Hong Kong internationally are containing the virus….but America is not ready. There are things that these countries are doing that appear to work (called evidence-based practices). Why can’t we do the same thing? Are we ready to adapt these methods to this country? Of course, it will take hard work and near total cooperation from the public to stay 6 feet apart from everyone else, not gather in groups of 3 or more, and really obey the stay at home restrictions. But it is better than sickness and death all around us, our doctors and hospitals overwhelmed with more patients than they can care for, and our parents and grandparents denied intensive care because there isn’t enough, and dying before they have to.
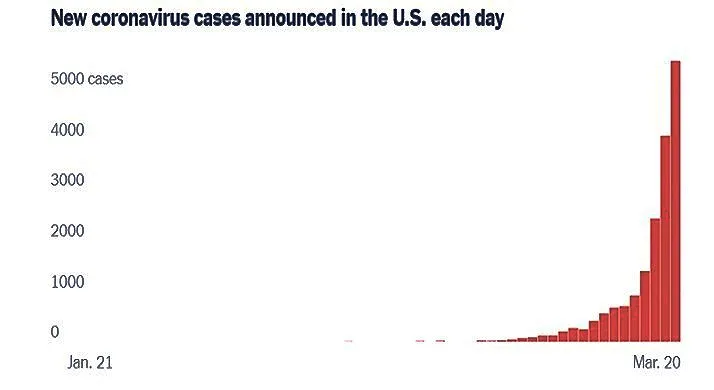
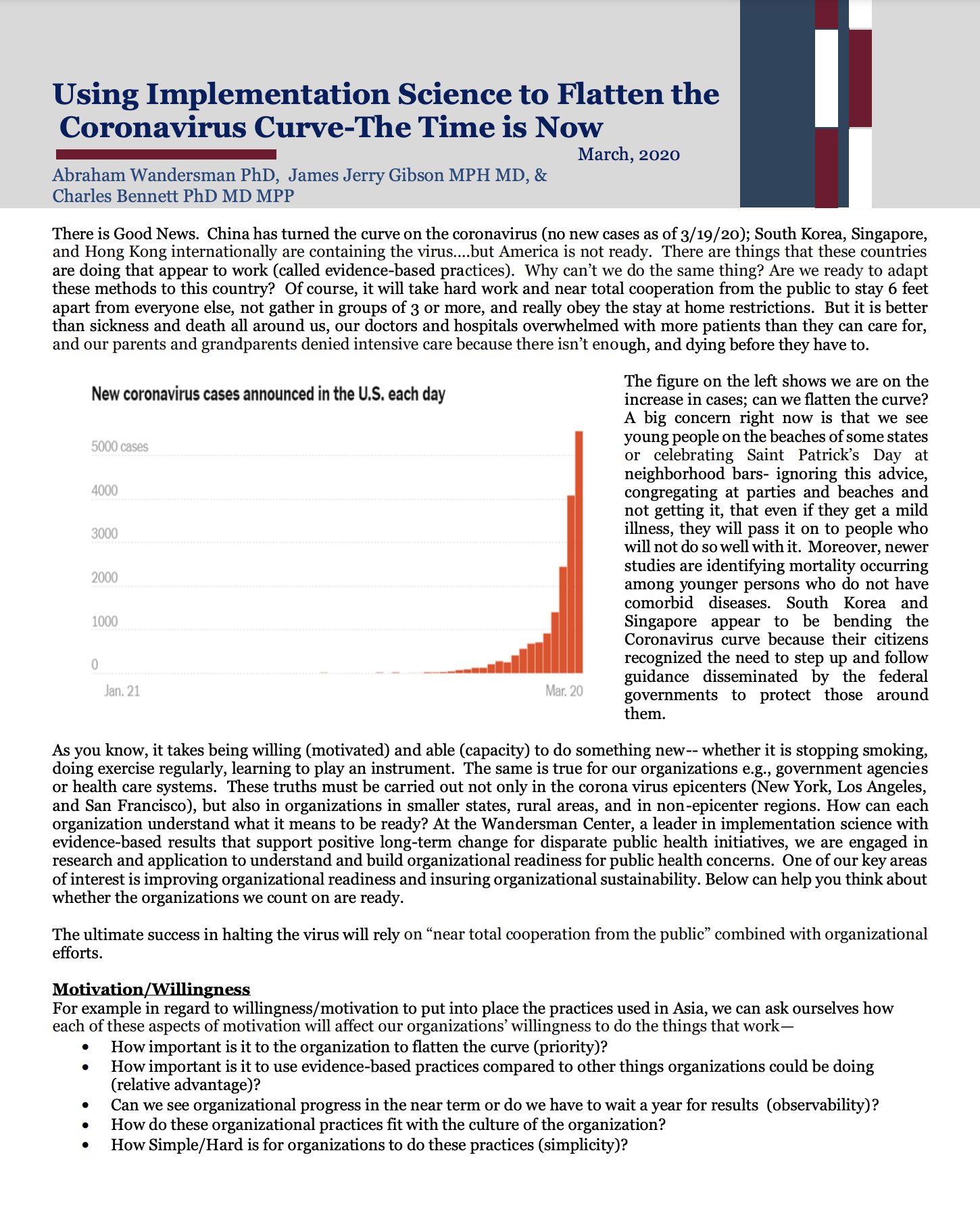
The figure above shows we are on the increase in cases; can we flatten the curve? A big concern right now is that we see young people on the beaches of some states or celebrating Saint Patrick’s Day at neighborhood bars- ignoring this advice, congregating at parties and beaches and not getting it, that even if they get a mild illness, they will pass it on to people who will not do so well with it. Moreover, newer studies are identifying mortality occurring among younger persons who do not have comorbid diseases. South Korea and Singapore appear to be bending the Coronavirus curve because their citizens recognized the need to step up and follow guidance disseminated by the federal governments to protect those around them.
As you know, it takes being willing (motivated) and able (capacity) to do something new– whether it is stopping smoking, doing exercise regularly, learning to play an instrument. The same is true for our organizations e.g., government agencies or health care systems. These truths must be carried out not only in the corona virus epicenters (New York, Los Angeles, and San Francisco), but also in organizations in smaller states, rural areas, and in non-epicenter regions. How can each organization understand what it means to be ready? At the Wandersman Center, a leader in implementation science with evidence-based results that support positive long-term change for disparate public health initiatives, we are engaged in research and application to understand and build organizational readiness for public health concerns. One of our key areas of interest is improving organizational readiness and insuring organizational sustainability. Below can help you think about whether the organizations we count on are ready.
The ultimate success in halting the virus will rely on “near total cooperation from the public” combined with organizational efforts.
Motivation/Willingness
For example in regard to willingness/motivation to put into place the practices used in Asia, we can ask ourselves how each of these aspects of motivation will affect our organizations’ willingness to do the things that work
- How important is it to the organization to flatten the curve (priority)?
- How important is it to use evidence-based practices compared to other things organizations could be doing (relative advantage)?
- Can we see organizational progress in the near term or do we have to wait a year for results (observability)?
- How do these organizational practices fit with the culture of the organization?
- How Simple/Hard is for organizations to do these practices (simplicity)?
CAPACITY/ABILITY Capacity/Ability
- How able are our organizations to do the practices that have been effective in China, Singapore, and Hong Kong?
- Do our organizational leaders have the knowledge and skills to do the practices (knowledge)?
- Do our organizations have a champion—an important leader who is insisting that these practices be done well (champion)?
- Are the organizations that are supposed to do the practices really supporting it e.g., with equipment, training, person power (supportive climate)?
- Are the relationships between different units in each organization coordinated (e.g., within the state Departments of Health, different units would need to work together to do the practice or in a hospital are the outpatient, emergency room, and in-patient units coordinated (Intra organizational relationships)?
- Are relationships between organizations in place to do the practice (e.g., between the Department of Health and first responders) (Interorganizational relationships)?
Organizations will have to be willing to change how they implement prevention and screening methods as they learn what is working and what is not. This is called “re-planning” and was used by General Dwight Eisenhower, who was aware of the first rule of disaster planning: “No Plan survives the first contact with the enemy unchanged.” An example today is the fact that many primary care doctors’ offices are not offering patients the Coronavirus test, because the health care system that they work for cannot obtain masks, gloves and gowns to protect nurses who obtain nasal swabs from patients. We are the middle of re-planning with soon to be FDA approved corona virus self-sampling efforts where the patient mails a swab of sputum to a central processing company. This is an example of how people and health care providers can work together (what Nobel Prize winners call co-production). Now that you have a clearer idea about what it means to be ready—we ask the question: Are organizations ready to take the lead in flattening the coronavirus curve?
Abraham Wandersman PhD, Distinguished Emeritus Professor of Psychology, the University of South Carolina. Dr. Wandersman directs the Wandersman Center, an internationally recognized organization based on implementation science that performs research and program evaluation on citizen participation in community organizations.
James J Gibson MD, MPH is a medical epidemiologist retired from the US Centers for Disease Control and Prevention. He is now consulting with the SC Department of Health and Environmental Control on the coronavirus and working part time lecturing at schools of Public Health in South Carolina and Georgia, and recently did part-time work on HIV Pre-Exposure Prophylaxis for South Carolina Department of Health and Environmental Control (SCDHEC). He retired as State Epidemiologist and Director of Disease Control from the South Carolina Department of Health and Environmental Controls CDHEC in 2012. He has also worked previously for the CDC and as an Associate Professor of Preventive Medicine at the University of South Carolina. He was a Peace Corps Volunteer in Malawi in 1964-66.
Charles L Bennett MD PhD MPP is the SmartState Chair and Director of the SmartState Center for Medication Safety and Efficacy at the University of South Carolina. He collaborated with the late Baruch Blumberg MD PhD, ’75 Nobel Prize in Medicine recipient in documenting the effectiveness of the World Health Organization’s hepatitis B eradication program was in decreasing the impact of hepatitis B in many Asian countries from 18% to 0.5% through nationwide vaccination programs.
End Notes / References
“NY Times” 3/19/20
“Before the Coronavirus Outbreak, A Cascade of Warnings Went Unheeded, Government Exercises, including a pandemic simulation last year, made it clear that the U.S. was not ready for a crisis like the coronavirus”. Re: “Halting Virus will Require Harsh Steps, Expert Says: Near Total Cooperation from Public is Key to Isolating Clusters of Infection.” (NYT, March 23, 2020).
Dymnicki, A., Bzura, R. Osher, D., Wandersman, A. Duplantier, D., Boyd, M. Cash, A. & Huthcison, L. (2019) Important implementation constructs for federal agencies in health and human service settings that are selecting, monitoring, and supporting grantees. Evidence and Policy. https://doi.org/10.1332/174426418X15409834211096
Hajjar,L.,Cook,B. S.,Domlyn,A.,Ray,K. A.,Laird,D.,& Wandersman,A.(2020).Readiness and relationships are crucial for coalitions and collaboratives: Concepts and evaluation tools. In A. W. Price, K. K. Brown, & S. M. Wolfe (Eds.), Evaluating Community Coalitions and Collaboratives. New Directions for Evaluation, 165, 103–122
Scaccia, J., Cook, B., Lamont, A., Wandersman, A., Castellow, J., Katz, J., & Beidas, R. (2015) A Practical implementation science heuristic for organizational readiness: R = MC2. Journal of Community Psychology. 43, 483-501.
Scott, V. C., Kenworthy, T., Godly-Reynolds, E., Bastien, G., Scaccia, J., McMickens, C., Rachel, S., Cooper, S., Wrenn, G., & Wandersman, A. (2017, April 10). The Readiness for Integrated Care Questionnaire (RICQ): An Instrument to Assess Readiness to Integrate Behavioral Health andPrimary Care. American Journal of Orthopsychiatry. Advance online publication.http://dx.doi.org/10.1037/ort0000270
The Research-to-Policy Collaboration (RPC) works to bring together research professionals and public officials to support evidence-based policy. Please visit their website to learn more.
Key Information
RPC Website
Research-to-Policy Collaboration
Publication DateMarch 1, 2020
Topic Area(s)Social Services, Violence and Victimization
Resource TypeWritten Briefs
Share This Page
There is Good News. China has turned the curve on the coronavirus (no new cases as of 3/19/20); South Korea, Singapore, and Hong Kong internationally are containing the virus….but America is not ready. There are things that these countries are doing that appear to work (called evidence-based practices). Why can’t we do the same thing? Are we ready to adapt these methods to this country? Of course, it will take hard work and near total cooperation from the public to stay 6 feet apart from everyone else, not gather in groups of 3 or more, and really obey the stay at home restrictions. But it is better than sickness and death all around us, our doctors and hospitals overwhelmed with more patients than they can care for, and our parents and grandparents denied intensive care because there isn’t enough, and dying before they have to.
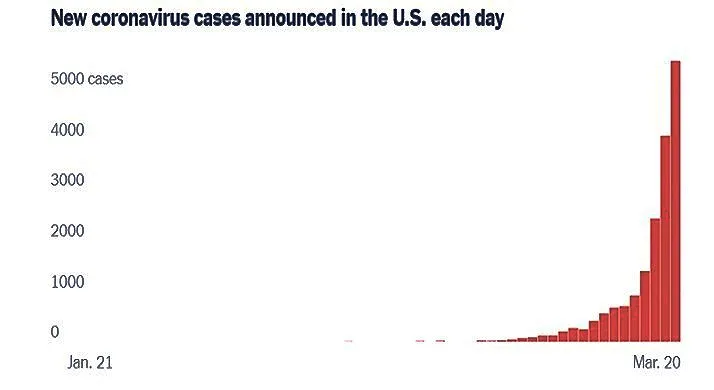
The figure above shows we are on the increase in cases; can we flatten the curve? A big concern right now is that we see young people on the beaches of some states or celebrating Saint Patrick’s Day at neighborhood bars- ignoring this advice, congregating at parties and beaches and not getting it, that even if they get a mild illness, they will pass it on to people who will not do so well with it. Moreover, newer studies are identifying mortality occurring among younger persons who do not have comorbid diseases. South Korea and Singapore appear to be bending the Coronavirus curve because their citizens recognized the need to step up and follow guidance disseminated by the federal governments to protect those around them.
As you know, it takes being willing (motivated) and able (capacity) to do something new– whether it is stopping smoking, doing exercise regularly, learning to play an instrument. The same is true for our organizations e.g., government agencies or health care systems. These truths must be carried out not only in the corona virus epicenters (New York, Los Angeles, and San Francisco), but also in organizations in smaller states, rural areas, and in non-epicenter regions. How can each organization understand what it means to be ready? At the Wandersman Center, a leader in implementation science with evidence-based results that support positive long-term change for disparate public health initiatives, we are engaged in research and application to understand and build organizational readiness for public health concerns. One of our key areas of interest is improving organizational readiness and insuring organizational sustainability. Below can help you think about whether the organizations we count on are ready.
The ultimate success in halting the virus will rely on “near total cooperation from the public” combined with organizational efforts.
Motivation/Willingness
For example in regard to willingness/motivation to put into place the practices used in Asia, we can ask ourselves how each of these aspects of motivation will affect our organizations’ willingness to do the things that work
- How important is it to the organization to flatten the curve (priority)?
- How important is it to use evidence-based practices compared to other things organizations could be doing (relative advantage)?
- Can we see organizational progress in the near term or do we have to wait a year for results (observability)?
- How do these organizational practices fit with the culture of the organization?
- How Simple/Hard is for organizations to do these practices (simplicity)?
CAPACITY/ABILITY Capacity/Ability
- How able are our organizations to do the practices that have been effective in China, Singapore, and Hong Kong?
- Do our organizational leaders have the knowledge and skills to do the practices (knowledge)?
- Do our organizations have a champion—an important leader who is insisting that these practices be done well (champion)?
- Are the organizations that are supposed to do the practices really supporting it e.g., with equipment, training, person power (supportive climate)?
- Are the relationships between different units in each organization coordinated (e.g., within the state Departments of Health, different units would need to work together to do the practice or in a hospital are the outpatient, emergency room, and in-patient units coordinated (Intra organizational relationships)?
- Are relationships between organizations in place to do the practice (e.g., between the Department of Health and first responders) (Interorganizational relationships)?
Organizations will have to be willing to change how they implement prevention and screening methods as they learn what is working and what is not. This is called “re-planning” and was used by General Dwight Eisenhower, who was aware of the first rule of disaster planning: “No Plan survives the first contact with the enemy unchanged.” An example today is the fact that many primary care doctors’ offices are not offering patients the Coronavirus test, because the health care system that they work for cannot obtain masks, gloves and gowns to protect nurses who obtain nasal swabs from patients. We are the middle of re-planning with soon to be FDA approved corona virus self-sampling efforts where the patient mails a swab of sputum to a central processing company. This is an example of how people and health care providers can work together (what Nobel Prize winners call co-production). Now that you have a clearer idea about what it means to be ready—we ask the question: Are organizations ready to take the lead in flattening the coronavirus curve?
Abraham Wandersman PhD, Distinguished Emeritus Professor of Psychology, the University of South Carolina. Dr. Wandersman directs the Wandersman Center, an internationally recognized organization based on implementation science that performs research and program evaluation on citizen participation in community organizations.
James J Gibson MD, MPH is a medical epidemiologist retired from the US Centers for Disease Control and Prevention. He is now consulting with the SC Department of Health and Environmental Control on the coronavirus and working part time lecturing at schools of Public Health in South Carolina and Georgia, and recently did part-time work on HIV Pre-Exposure Prophylaxis for South Carolina Department of Health and Environmental Control (SCDHEC). He retired as State Epidemiologist and Director of Disease Control from the South Carolina Department of Health and Environmental Controls CDHEC in 2012. He has also worked previously for the CDC and as an Associate Professor of Preventive Medicine at the University of South Carolina. He was a Peace Corps Volunteer in Malawi in 1964-66.
Charles L Bennett MD PhD MPP is the SmartState Chair and Director of the SmartState Center for Medication Safety and Efficacy at the University of South Carolina. He collaborated with the late Baruch Blumberg MD PhD, ’75 Nobel Prize in Medicine recipient in documenting the effectiveness of the World Health Organization’s hepatitis B eradication program was in decreasing the impact of hepatitis B in many Asian countries from 18% to 0.5% through nationwide vaccination programs.
End Notes / References
“NY Times” 3/19/20
“Before the Coronavirus Outbreak, A Cascade of Warnings Went Unheeded, Government Exercises, including a pandemic simulation last year, made it clear that the U.S. was not ready for a crisis like the coronavirus”. Re: “Halting Virus will Require Harsh Steps, Expert Says: Near Total Cooperation from Public is Key to Isolating Clusters of Infection.” (NYT, March 23, 2020).
Dymnicki, A., Bzura, R. Osher, D., Wandersman, A. Duplantier, D., Boyd, M. Cash, A. & Huthcison, L. (2019) Important implementation constructs for federal agencies in health and human service settings that are selecting, monitoring, and supporting grantees. Evidence and Policy. https://doi.org/10.1332/174426418X15409834211096
Hajjar,L.,Cook,B. S.,Domlyn,A.,Ray,K. A.,Laird,D.,& Wandersman,A.(2020).Readiness and relationships are crucial for coalitions and collaboratives: Concepts and evaluation tools. In A. W. Price, K. K. Brown, & S. M. Wolfe (Eds.), Evaluating Community Coalitions and Collaboratives. New Directions for Evaluation, 165, 103–122
Scaccia, J., Cook, B., Lamont, A., Wandersman, A., Castellow, J., Katz, J., & Beidas, R. (2015) A Practical implementation science heuristic for organizational readiness: R = MC2. Journal of Community Psychology. 43, 483-501.
Scott, V. C., Kenworthy, T., Godly-Reynolds, E., Bastien, G., Scaccia, J., McMickens, C., Rachel, S., Cooper, S., Wrenn, G., & Wandersman, A. (2017, April 10). The Readiness for Integrated Care Questionnaire (RICQ): An Instrument to Assess Readiness to Integrate Behavioral Health andPrimary Care. American Journal of Orthopsychiatry. Advance online publication.http://dx.doi.org/10.1037/ort0000270
The Research-to-Policy Collaboration (RPC) works to bring together research professionals and public officials to support evidence-based policy. Please visit their website to learn more.
Key Information
RPC Website
Research-to-Policy Collaboration
Publication DateMarch 1, 2020
Topic Area(s)Social Services, Violence and Victimization
Resource TypeWritten Briefs
Share This Page
LET’S STAY IN TOUCH
Join the Evidence-to-Impact Mailing List
Keep up to date with the latest resources, events, and news from the EIC.